What Is TMS Therapy (Transcranial Magnetic Stimulation)?
- The Summit

- Nov 25, 2025
- 4 min read
Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation therapy that uses magnetic pulses to stimulate nerve cells in specific brain regions that regulate mood and cognition. The technique was pioneered in the 1980s and first applied for clinical treatment in depression when the U.S. Food and Drug Administration (FDA) approved TMS for Major Depressive Disorder (MDD) in adults in 2008.

History and FDA Approval of TMS Therapy
The history of TMS can be traced to 1985 when Anthony Barker developed the first working magnetic stimulation device for use on the human brain. Over the following decades, researchers refined the method and in 2008 the FDA cleared the first device for treatment-resistant depression. Since then, TMS has expanded into other device models and indications.
Today, TMS is recognized as a legitimate option for people who’ve not achieved adequate relief from antidepressants or psychotherapy, and its evidence base continues to grow.
How Does TMS Therapy Work?
Here’s how the therapy is delivered and why it may help:
A magnetic coil is placed against the scalp, usually over the dorsolateral prefrontal cortex (DLPFC) — a brain region linked to mood regulation. Cambridge University Press & Assessment.
The device sends brief electromagnetic pulses that penetrate the skull and induce small electric currents in underlying brain tissue. These currents activate neurons and modulate neural circuits. College of Medicine - Tucson
Repeated stimulation over days or weeks is thought to strengthen synaptic connectivity, adjust neurotransmitter systems (serotonin, dopamine, norepinephrine), and improve neural network efficiency in mood-control circuits. College of Medicine - Tucson
The non-invasive nature means no surgery, implants, or anesthesia are required — you remain awake and can resume normal activities after each session.
Because TMS directly targets brain circuits rather than relying solely on systemic medications, it offers an alternative path when medication response is inadequate.

Is TMS Therapy Safe?
What are the Pros and Cons of TMS?
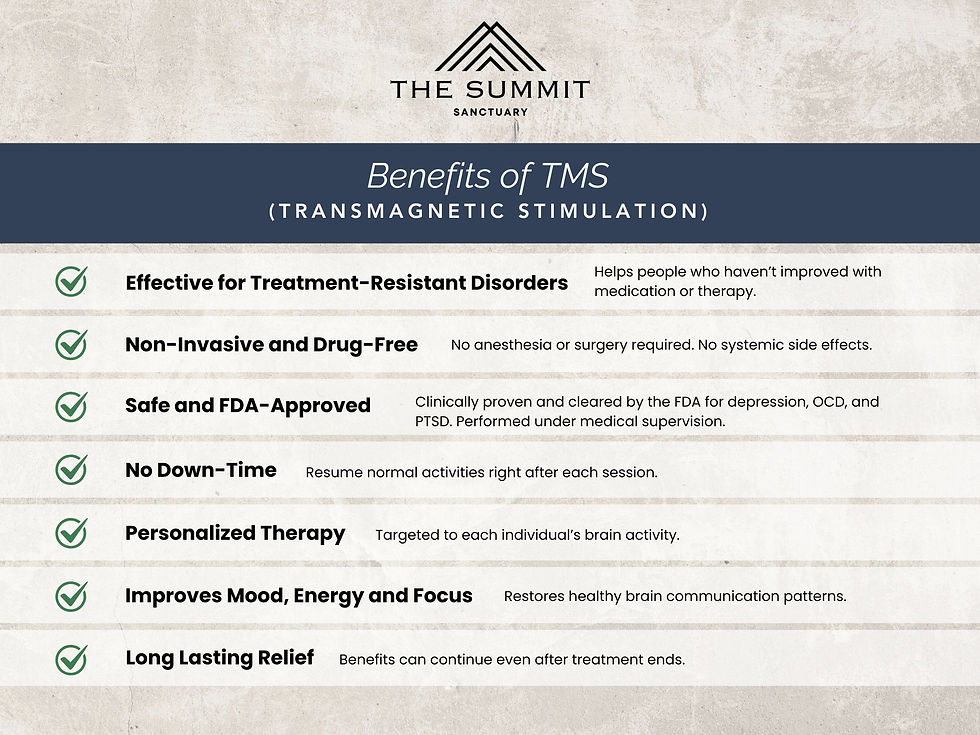
Pros:
Non-surgical, no anesthesia required.
Minimal systemic side-effects compared to many antidepressant medications (no sedation, few drug interactions).
Good safety profile: seizures are extremely rare when protocols are followed. Wikipedia+1
Increasingly effective in treatment-resistant cases: literature reports ~50–60% respond and ~30–35% achieve remission in some studies. Verywell Health+1
Cons:
Treatment requires commitment (daily sessions over several weeks).
Some scalp discomfort, headache or twitching may occur during early treatments.
TMS is not appropriate for everyone — individuals with metal implants in or near the head, certain seizure disorders, or active psychosis may not be safe candidates.
Although effective, TMS is not guaranteed — some patients may not respond or may require maintenance sessions.
In short:
TMS is considered safe and well-tolerated for appropriately screened individuals, but like all treatments, it has limitations and must be administered by experienced providers.
Is TMS Therapy Covered by Insurance?
Insurance coverage for TMS has expanded significantly as its evidence base has grown. Many commercial, Medicare, and Medicaid plans do cover TMS for MDD when certain criteria are met:
A diagnosis of MDD (or other cleared indication)
Documentation of prior failed antidepressant medication trials
Evidence of psychotherapy attempts
Treatment by a qualified, device-certified TMS provider
Because policies vary, you should confirm with your insurer and ask whether the clinic is in-network, what prior authorization is required, and what your out-of-pocket obligations will be.
Given the upfront cost of TMS (often several thousand dollars without insurance), having coverage makes a meaningful difference. If you’d like, we can provide a list of insurers who currently cover TMS in your state.

Does TMS Therapy Help with Anxiety?
And What Other Conditions Can TMS Treat?
Yes—while TMS is most commonly applied to depression, there is growing evidence that it can also help with symptoms of anxiety and other conditions:
In individuals treated for MDD with comorbid anxiety, TMS has shown meaningful reductions in anxiety symptoms as mood improves. For example, a recent dataset in adolescents treated with Deep TMS showed a 66.1 % response rate and accompanying reductions in anxiety scores. markets.businessinsider.com
Beyond anxiety, TMS has been FDA-cleared for Obsessive-Compulsive Disorder (OCD) and smoking cessation, and is being studied for migraines, PTSD, chronic pain, epilepsy and more. Carlat Publishing+1
So while TMS is not a “first-line” anxiety treatment in the absence of depression, for many patients with overlapping depression and anxiety, it can deliver dual benefit.
What Does TMS Therapy Look Like?
Here’s a typical course:
Initial evaluation and screening (including medical/psychiatric history, safety review).
Mapping and motor-threshold determination: the first session involves locating the optimal coil position and energy level.
Daily treatment sessions (Monday through Friday) over 4 to 8 weeks, each session lasting ~20–45 minutes (varies by protocol).
During each session you sit in a comfy chair, a coil placed on your scalp, you hear clicking and feel tapping — you stay fully awake and alert.
After each session, you resume normal daily activities. No recovery time required.
After completion of the acute phase, you may undergo maintenance sessions occasionally or continue with medication and therapy in combination.
Patient experience often includes a gradual lifting of mood, increased energy, improved focus, better sleep, and rekindled interest in activities.

Where Can I get TMS Therapy?
You should seek care at a clinic or healthcare facility that provides certified TMS treatment under oversight of a physician (often a psychiatrist) and trained technicians.
Steps:
Ask your mental health provider for a TMS referral if you’ve failed to respond to conventional treatments.
Contact a local TMS provider to verify:
Their device is FDA-cleared
They are in-network with your insurance (or will bill your plan)
They coordinate insurance prior authorization
They provide you with a clear treatment schedule, costs and expectations
Once approved, schedule your treatment calendar and arrange for transportation/availability for the full course.
Local centers often advertise “treatment-resistant depression” or “neuromodulation therapy” and will be happy to speak with you about your eligibility.

Closing: TMS Therapy at The Summit Sanctuary
At The Summit Sanctuary, we offer compassionate, cutting-edge TMS therapy in a comfortable, patient-centred setting. Our TMS program is overseen by board-certified psychiatrists and operated by a dedicated team of neuromodulation specialists. We understand the frustration of living with depression or anxiety that hasn’t responded to standard treatments. That’s why we integrate TMS as part of a whole-person plan — combining personalized neuromodulation, psychotherapy, lifestyle support, and ongoing follow-up.

If you’re ready to explore whether TMS may be the right next step, we invite you to contact The Summit Sanctuary for a no-obligation consultation. Let us help you chart your path to relief, restoration, and renewed hope.

















TMS is an FDA-approved, non-invasive treatment that uses magnetic LifeQuality TMS pulses to stimulate specific areas of the brain responsible for mood regulation